Oxcarbazepine
"150mg oxcarbazepine visa, symptoms sinus infection."
By: Lars I. Eriksson, MD, PhD, FRCA
- Professor and Academic Chair, Department of Anaesthesiology and Intensive Care Medicine, Karolinska University Hospital, Solna, Stockholm, Sweden
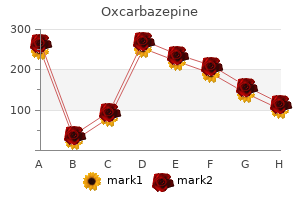
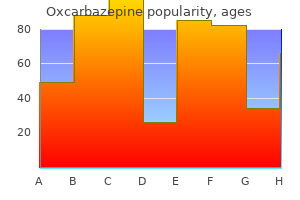
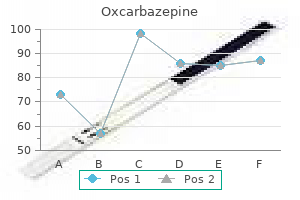
As the muscle is stretched from its slack length (the length at which no force is generated) medicine youth lyrics cheap oxcarbazepine 300mg line, both the resting (end-diastolic) tension and the peak (end-systolic) tension increase medicine valley high school oxcarbazepine 600mg sale. The end-diastolic force-length relationship is non-linear and exhibits a shallow slope at small lengths and a steeper slope at larger lengths medicine university generic 300mg oxcarbazepine otc, which is a reflection of the non-linear mechanical restraints imposed by the sarcolemma and extracellular matrix to treatment uveitis cheap 150mg oxcarbazepine mastercard prevent overstretch of the sarcomeres. End-systolic force increases with increasing muscle length to a much greater degree than does end-diastolic force. The difference in force at end-diastole as compared with end-systole increases as muscle length increases and indicates a greater amount of developed force as the muscle is stretched. This fundamental property of cardiac muscle is called the Frank-Starling law of the heart in recognition of its two discoverers. If a drug increases the amount of calcium released to the myofilaments (for example, epinephrine, which belongs to a class of drugs referred to as inotropic agents), the end-systolic force-length relationship will be shifted upward and at any given length the muscle can generate more force. Inotropic agents typically do not affect the end-diastolic force-length relationship. In view of the prominent effect of muscle length on force generation, the intrinsic strength of cardiac muscle, commonly referred to as muscle contractility, should be indexed by the end-systolic force-length relationship and not simply by peak force generation. Muscle length and the force generated by muscles in the walls of the ventricles are interrelated with the volume and pressure within the chambers. It is intuitively clear that as ventricular chamber volume varies, so too do muscle and sarcomere lengths. Ventricular pressure is related to the force within the walls and the geometry of the chamber. From this equation it is clear that chamber pressure depends on both tension and muscle length (because muscle length is related to chamber volume, which is related to chamber radius). Because of the complex structure and geometry of the right ventricle, no simple analytic equation can describe this interrelationship; however, the underlying principle is the same. Just as end-systolic and end-diastolic force-length relationships can be used to characterize the systolic and diastolic properties of cardiac muscle fibers, so too can end-systolic and end-diastolic pressure-volume relationships be used to characterize the peak systolic and end-diastolic properties of the ventricular chambers. Analogous to muscle, the end-diastolic pressure-volume relationship is non-linear, with a shallow incline at low pressures and a steep rise at pressures in excess of 20 mm Hg. However, the end-systolic pressure-volume relationship is typically linear, and as for muscle, ventricular pressure-generating capability is increased as ventricular volume is increased. Also analogous to muscle, the end-systolic pressure-volume relationship is used to index ventricular chamber contractility. Because the end-systolic pressure-volume relationship is roughly linear, it can be characterized by a slope and volume axis intercept. The slope of the line, which has units of myocardial stiffness or volume elastance (mm Hg/mL) is called Ees (end-systolic elastance), and the volume axis intercept (analogous to slack length of the muscle) is referred to as V0. When muscle contractility is increased (for example, by administration of an inotropic agent), the slope of the end-systolic pressure-volume relationship (Ees) increases, whereas little change occurs in V0 (discussed further below). The heart beats roughly once every second and repeatedly cycles through a sequence of hemodynamic events that can be divided into four phases. This cycle can be summarized by tracking the time course of change in ventricular pressure and volume along with atrial and aortic pressures in relation to events noted on the electrocardiogram. At end-diastole, ventricular pressure is at its resting level (end-diastolic pressure) and ventricular volume is at its maximal value (end-diastolic volume). Aortic pressure declines gradually during this period as the blood ejected into the aorta during the prior ventricular contraction discharges to the peripheral circulation. Just before the onset of ventricular systole, atrial contraction provides a final boost to ventricular volume. As ventricular contraction begins about 120 milliseconds later, pressure rises inside the ventricular chamber and exceeds the pressure in the atrium; this pressure differential causes the mitral valve to close. Ventricular pressure is still less than that of the aorta, so the aortic valve remains closed. Because both valves are closed, no blood enters or leaves the ventricle during this time; this first phase is called isovolumic contraction. As systole progresses, ventricular pressure eventually exceeds that of the aorta, so the aortic valve opens.

The main goals of therapy should be to brazilian keratin treatment generic oxcarbazepine 300mg (1) establish the bladder as a urine storage organ without causing renal injury and (2) provide a mechanism for bladder emptying that is acceptable to medicine klimt oxcarbazepine 150 mg without prescription the patient medicine university order 300 mg oxcarbazepine with amex. Patients fall into two categories treatment quadriceps pain order 150 mg oxcarbazepine, those with atonic bladders secondary to lower motor neuron injury and those with unstable bladder function from upper motor neuron disease. The neurogenic bladder seen in patients with diabetes mellitus is usually the result of lower motor neuron disease. Requesting these patients to void at regular intervals achieves satisfactory emptying of the bladder. Occasionally, these individuals respond to cholinergic agents such as bethanechol chloride (Urecholine). The best treatment of patients with significant residual urine and recurrent urosepsis is to establish clean, intermittent, regular self-catheterization. The goal is to catheterize four or five times per day so that the amount of urine drained from the bladder does not exceed 400 mL. This technique may be successful but requires patient acceptance and adequate training. In patients with a hypertonic bladder, the major goal is to improve its storage function. In all patients with neurogenic bladders, long-term use of indwelling catheters should be avoided if possible because of the risk of infection and other complications. This diuresis is characterized by the excretion of large amounts of sodium, potassium, magnesium, and other solutes. Although usually self-limited, the losses of solutes and water may result in hypokalemia, hyponatremia or hypernatremia, hypomagnesemia, and marked volume depletion. In many patients, a brisk diuresis after relief of obstruction may represent a physiologic response to the expansion in extracellular fluid volume that occurred during the period of obstruction. This post-obstructive diuresis is appropriate and does not compromise the volume status of the patient. Post-obstructive diuresis in this setting can be prolonged 605 by overzealous replacement of salt and water after the relief of obstruction. Fluid replacement is justified only when excessive losses of sodium and water are inappropriate for the volume status of the patient and are presumably due to an intrinsic tubular defect in sodium and water reabsorption. Intravenous fluid administration may be necessary, but urinary losses should be replaced only to the extent necessary to prevent extracellular fluid volume contraction or electrolyte imbalance. The return of renal function after relieving obstruction is variable and influenced by the severity and duration of the obstruction. Other events that condition the degree of recovery of renal function include the presence of infection, stones, pre-existing renal disease, and/or the underlying cause of the obstruction. Renal cortical thickness is a prognostic indicator of residual renal function in patients with chronic hydronephrosis. A detailed chapter on pathogenesis and clinical and diagnostic issues in obstructive nephropathy; numerous references. Chesney Renal tubular disorders represent a group of conditions in which the renal tubular reabsorption of either ions or organic solutes is diminished, resulting in excessive amounts of either substance in the urine. The functions of each segment will influence the type of substance lost as well as the rate of loss. As noted in Chapter 101, the proximal nephron is responsible for reclaiming most of the filtered glucose, amino acids, uric acid, phosphate, bicarbonate, and low-molecular-weight proteins. The distal nephron (including the cortical and medullary collecting ducts), under the influence of aldosterone, reabsorbs the final amount of sodium and secretes hydrogen and potassium ions. The terminal collecting ducts are influenced by antidiuretic hormone to permit water reabsorption and hence lead to urinary concentration. Many tubular disorders are inherited and appear to involve the loss or formation of a defective transport protein ("carrier") and represent an inborn error of transport. Because many of these transporter proteins and channels have been cloned, the precise genetic defect of many of thse conditions can now be understood more completely. These conditions include (1) a single selective transport defect, (2) a class-specific defect. Luminal, intracellular, or peritubular components of the net transport process can be affected in each situation. Several of the more usual transport defects of individual nephron segments are described here. Urinary wastage of bulk quantities of these solutes implies a disorder of proximal tubular function.
This observation is controversial symptoms with twins cheap oxcarbazepine 300 mg on line, and animal experiments have yielded conflicting results medications of the same type are known as buy oxcarbazepine 300 mg overnight delivery. Although some initial clinical studies reported improved outcomes when oxygen delivery was increased symptoms in early pregnancy cheap 600 mg oxcarbazepine fast delivery, subsequent larger clinical trials comparing conventional strategies with strategies designed to treatment h pylori 600 mg oxcarbazepine amex increase oxygen delivery to a supranormal range have failed to demonstrate a survival advantage for the supranormal approach. Some studies suggest that pretreatment of critically ill surgical patients with supranormal oxygen delivery may provide some benefit, but further studies will be necessary to resolve these controversial findings. First, the patient usually manifests symptoms and signs related to the primary focus of infection. If it is pneumonia, then the patient usually has cough, dyspnea, and productive sputum; if a urinary tract infection is the focus, then flank pain and dysuria would be expected. A careful history, physical examination, and directed imaging and laboratory studies will reveal the probable infectious focus in most patients. However, elderly, debilitated, and immunosuppressed patients may not exhibit the usual localizing clinical signs. In some patients, especially those with severe neutropenia, no site is identified. Second, patients usually manifest one or more signs of the systemic inflammatory response. Elderly patients may present with tachypnea-induced respiratory alkalosis and mental status changes as the only signs of sepsis. Third, septic patients may develop evidence of shock, such as hypotension, lactic acidemia, and progressive organ system dysfunction. The diagnosis of sepsis is confirmed by culturing pathogenic organisms from blood or from the likely site of infection. Blood cultures are positive in only 40 to 60% of patients with clinical manifestations of septic shock, probably owing to the intermittent nature of the bacteremia and the high incidence of prior antibiotic administration. A Gram stain from an abscess, empyema, or other usually sterile site can provide invaluable early diagnostic information. First, the infection site can be eradicatedwith antimicrobials, surgical drainage, or both. Second, the serious disturbances in cardiovascular, respiratory, and other organ system 511 Figure 96-3 Algorithm for diagnostic evaluation and management of sepsis and septic shock. Shock secondary to sepsis is a very major disease that should be treated aggressively. When the diagnosis is seriously entertained, blood cultures (usually three) and cultures of relevant body fluids and exudates should be obtained rapidly. Several large retrospective trials have provided convincing evidence that early appropriate antimicrobial therapy. A broad-spectrum regimen with activity against gram-positive and gram-negative organisms should be chosen. Generally, drugs should be administered intravenously at maximum recommended dosages, and bactericidal agents are preferred over bacteriostatic agents. Many physicians favor using at least two effective antimicrobial agents in neutropenic patients with gram-negative pneumonia and a two-drug synergistic combination when treating serious enterococcal infection (see Chapter 314). Anaerobes are likely pathogens in intra-abdominal infections, aspiration pneumonia, and abscesses. Intravascular catheter infection should raise the possibility of methicillin-resistant staphylococcal infection and the need for vancomycin therapy. In up to one third of patients, especially those who are neutropenic, no organism or source will be identified. Such patients require a broad-spectrum regimen effective against gram-positive, gram-negative, and anaerobic organisms such as (1) vancomycin, gentamicin, and metronidazole or (2) ceftazidime and gentamicin. The need for early antifungal therapy with amphotericin B should be considered in neutropenic, immunosuppressed patients and in those unresponsive to antibacterial regimens. Before the general availability of intensive care units, gram-negative bacteremic shock had a higher than 90% mortality. Now, about 50% of such patients survive, largely because of treatment in intensive care units, in which cardiac rhythm, blood pressure, cardiac performance, oxygen delivery, and metabolic derangements can be monitored and abnormalities can be corrected. Although no prospective trial has evaluated outcomes with and without intensive care unit support, two retrospective studies have reported a significantly reduced mortality in septic shock when patients were managed with aggressive hemodynamic support by critical care personnel.
Syndromes
- Fever and chills
- You are still growing
- Worsening of a clot in the leg vein
- Narrowing of the bile ducts from scarring
- Irritability
- Can increase the chance for dehydration (not enough fluids in the body) and loss of calcium
- Weakened immune system
- Hypospadias [the opening of the penis is somewhere other than at the tip; in females, the urethra (urine canal) opens into the vagina]
However treatment impetigo order oxcarbazepine 150 mg free shipping, one can see platelet microemboli and vascular mural thrombosis medicine qid buy cheap oxcarbazepine 300mg on-line, which are of diverse age and indicate repetitive thrombotic phenomena initiated by dynamic changes in complicated atherosclerotic plaques treatment laryngomalacia infant discount oxcarbazepine 600mg amex. Pathophysiology the right and left coronary arteries arise most commonly independently from individual ostia associated with right and left aortic valve cusps medicine vicodin buy cheap oxcarbazepine 150 mg online. The right coronary artery generally supplies the right ventricle, the posterior third of the interventricular septum, the inferior wall (diaphragmatic surface) of the left ventricle, and a portion of the posterior wall of the left ventricle (via the posterior descending branch). When the posterior descending coronary artery that supplies the posterior interventricular septum arises from the left circumflex artery, the circulation is called left dominant. More often, the posterior descending artery arises from the right coronary artery (right dominant circulation). Another right coronary artery branch (in 55% of subjects) supplies the sinus node. However, markedly impaired left ventricular function with pulmonary congestion or edema indicative of extensive injury and intraventricular conduction defects, such as hemiblock, is more typical of left coronary artery occlusion. If coronary recanalization is not induced relatively promptly (spontaneously, mechanically, surgically, or with fibrinolytic drugs), regional myocardial perfusion may not be sustained despite restoration of patency (the "no-reflow" phenomenon) because of endothelial cell swelling, presence of platelet and leukocyte plugs, or complement-mediated microvascular inflammation. In addition to hypoxia, decreased removal of noxious metabolites, including potassium, 306 calcium, amphiphilic lipids, and oxygen-centered free radicals, impairs ventricular performance and may evoke lethal arrhythmias. Inflammation of endocardial surfaces and stasis associated with dyskinesis can lead to ventricular mural thrombi. Epicardial inflammation may initiate pericarditis, which is seen with more than 20% of Q-wave infarcts. Even transitory deprivation of oxygen and accumulation of metabolites promptly cause diminished diastolic relaxation, abnormal regional systolic contractile function and wall thickening, abnormal wall motion, diminished cardiac cycle-dependent variation of backscattered ultrasound, and, if extensive, diminished stroke volume. Restoring perfusion may promptly restore function of myocardium that exhibits decreased function because of decreased perfusion ("hibernating" myocardium). Often, however, impaired function persists for some period of time after blood flow is restored and before the myocardium recovers ("stunning"). In general, hypokinesis and akinesis reflect the locus and extent of myocardial injury. Clinically, aneurysms may be recognized only later, manifested by heart failure, recurrent ventricular arrhythmia, or recurrent emboli. As left ventricular end-diastolic volume and pressure increase because of impaired regional contractility and relaxation, intramural diastolic ventricular pressure increases and myocardial perfusion declines. Peripheral arterial vasoconstriction and systemic venous constriction can no longer offset declining stroke volume, and blood pressure falls. Normally perfused zones initially may exhibit compensatory hyperkinesis with excessive wall thickening in systole. However, as the heart dilates over a period of 24 to 48 hours, hyperkinesis regresses. As the infarct thins and shrinks, and if infarct expansion does not predominate, ventricular dilatation may regress, and diastolic cardiac and pulmonary pressures may return toward normal. Acute right ventricular dysfunction diminishes cardiac output disproportionally to left ventricular injury. High-grade bradyarrhythmias are common, including those resulting from third-degree heart block. Occasionally, profound arterial oxygen desaturation can develop because of augmented right atrial pressure and right-toleft shunting through a patent foramen ovale. The hemodynamic changes resemble many of those seen with pericardial constriction or tamponade (see Chapter 65). Initially, compromised cardiac output is maintained by the combination of increased heart rate and ventricular dilatation with recruitment of the Frank-Starling mechanism. As healing progresses and the right ventricle becomes less compliant, its conduit function is restored, permitting maintenance of cardiac output at the expense of augmentation of right ventricular filling pressure. Augmentation of pulmonary venous pressure may cause diminished pulmonary compliance, dyspnea, pulmonary vascular redistribution (detectable radiographically), interstitial and alveolar pulmonary edema, respiratory decompensation, and hypoxemia. Coupled with dyspnea in the elderly, it may be manifested only as confusion and combativeness. Increased sympathoadrenal tone reflected by markedly elevated plasma catecholamine levels and adrenocortical stimulation may be prominent as well.
Order oxcarbazepine 600 mg visa. 7 Signs Your Upper Respiratory Infection Is Actually Pneumonia.
References:
- https://scholarspace.manoa.hawaii.edu/bitstream/10125/50957/1/2015-05-phd-baker_r.pdf
- https://parasitesandvectors.biomedcentral.com/track/pdf/10.1186/s13071-019-3407-x.pdf
- https://www.toxpath.org/docs/SSNDC/EndocrineNonprolifRat.pdf
- https://www.opm.gov/healthcare-insurance/healthcare/plan-information/plan-codes/2020/brochures/73-004.pdf





